Each of us doing five easy actions might cut the risk and size of the COVID-19 pandemic by more than half
-
-
-
-
J. Bughin
Dr Jacques Bughin, UN consultant, Solvay Business School ULB, Portulans Institute and G20Y, former Director McKinsey Global Institute, and senior partner McKinsey & Company.
- Introduction
- A game plan in 5 actions
- The baseline of those 5 actions during outbreak: flattening the curve
- The aggregate picture
- What else to do
1. Introduction
March 12
The risk of a viral outbreak turning into a pandemic has become a reality for COVID-19, affecting to date more than hundred countries, and with a large concentration of known contaminated people in China, Italy, Iran and South Korea among others. People stress might remain imminent, as pharmaceutical responses, (be it an antiviral method for infected individuals, or be it a new type of vaccines), are largerly absent, or will take months to be developed.
As we discussed in previous articles (available here), it is rather crucial to act fast, due to large attack rates linked to influenza type of viruses. In fact, we have estimated form our own model of viral diffusion that one to two weeks delay in acting may easily create a multiple increase in the rate of the virus fatalities, a few weeks later.
Hopefully, we have shown that there are some proven, non pharmaceutical techniques, to curb a pandemic, even if some can create either large social disruption and/or are very costly from an economic perspective, such as school and work closing. Some can be relatively easy to do, e.g. hand washing, and may require not much, but more attention from ourselves, to perform systematically.
We herewith review an extensive set of academic papers, through Google Scholar, as well as academic journals, to provide a high level estimate of base line of non pharmaceutical actions, and how much more we should be doing to play our part in curbing the outbreak. Here are the findings:
2. A game plan in 5 actions
Wash your hands systematically please
Washing hands with soap is rather effective as a way to limit many types of infection if used systemically. For example, it decreases the risk of getting diarhhea by 25% to 40%.1
Regarding influenza, the findings on reducing disease occurrence are slightly lower or in the same ball park than/as diarhhea. On average, hand washing reduces the risk by 20% to 30% of getting influenza. The 5% most lucky ones may be reducing the risk by as much as 50% but the less 5% lucky ones, might not get anything from washing (versus non washing). It does not stop here. If the personal contact is at high risk of having infected, or the surface is contaminated, washing hands can double the pay off, with an average 40 to 50% % reduction in the risk of catching influenza.
As said, this is about washing your hands a) with soap, and b) systematically. Washing without soap strikes half the success rate, and the washing effect on risk reduction is roughly linear with the frequency of washing your hands.
What happens then if no soap? An alternative can be to use hand sanitizers. Even if there is large uncertainty in their potential, it looks like this is like a great, yet imperfect alternative, to hand washing with soaps, with roughly on average, 80% effectiveness of soap.
Are we really doing the washing hands thing? Research reports that, in a few years back, we were not good at it. In fact, worldwide, less than 20% of people seem to wash their hands with soap after going to toilets. In low- and middle-income regions, the rate was as low as between 5% and 25% of handwashing (remember that poor income countries have limited amount of toilets, and a fortiori, no water). Between 48% and 72% in high-income countries do wash their hands after going to toilets (see Freeman above). We also have a real gender issue: recent research with real tracking tools suggests that about 40% do wash their hands in UK, for about close to 70% for ladies.2
The fear of pandemic makes people change behavior, but not at the scale hoped. Roughly 30% to 40% extra people are typically reporting to wash their hands versus periods without influenza. This behavioral change is higher for children, women and families living in large cities, and for people being sick (65% more).3
Likewise, roughly half of those people washing their hands, do it rather frequently, up to 10 times a day.
Wear a mask
Asians have been using face masks extensively during outbreaks, and we saw some of them recently wearing goggles. Regarding masks, the use seems to be much more effective in the case of healthcare workers, possibly an average as good as 50% protection. This protection is not necessarily as large in other parts of the populatios, with 20% reduction according to recent WHO estimates. This is presumably because the extent of protection is likely to increase with its frequency of use, and the use and frequency of masks use is not that large. In fact, it is reported that the systematic use of mask is twice more effective at reducing the risk of being caught with the virus, than for irregular users.
Mask usage is also not that frequent in our population, in the course of recent, mild, influenza, roughly 5% (20%) of Western European people had used masks at start (peak) transmission and roughly half of them did this in fear of catching the virus, while the other half did it to protect their relatives based on their illness. During the H1N1 outbreak in 2019 in Hong Kong, roughly 25% of the inhabitants use to wear masks, but the percentage raised to 80% when going into public spaces.4
The average time a day wearing the mask is large, up to 4 hours, in the home, and is thus likely effective.
Ventilate : Always good to have a breath of fresh air
Another possible action is to increase ventilation of close spaces. The WHO reports on studies claiming that tripling the ventilation rate could reduce the peak infection rate by 30%. This however is simulation based, and relies on the crucial twin hypothesis of equal contribution of airborne and close contact transmission, and air condition change from once a day to 9 times a day. On average, 40% of infections may happen in close settings, yet typical research suggests that less than 20% of home owners leave windows open during sleep and less than 50% change air conditioning more than once a day.5 The behavior increases by 40% during risk of virus infection.
Do stay confined, if not well
Remain at home, or quarantined, may seem a logical step when there is a virus outbreak. However, there are multiple reasons why people do not do it, etiher because, despite having the symptoms, they do not feel that bad, because of peer pressure at work, because they do not have health insurance, etc.
Every year, it seems, a small, but material portion of workers or school kids keep their habits even if becoming sick from influenza; in the US, for example, 1 person out of 3 would still go to work in the private sector (10% in public sector). About 90% of kids will go to school while being sick too. If the disease infection rate per contact is 15% for influenza, and that the sick person makes 3 close contacts per day, and up to 6 in one week, the infected person may be responsible for one extra person sick in one week. This has led researchers in the US to say that non confinement is possibly half the causes of the flu pandemic attack rate.
During serious influenza, like H1N1, or a COVID-19 type, the rate of absence not only increases, but also the portion of sick workers coming to work decline, in the range of 30% to 50% versus normal infleunza, according to multiples studies.6
Limit close contacts
We already mentioned in a previous article that one key driver of mitigating a pandemic, is through a reduction of contacts, so called social distancing. Major policies enforcements exist for this, such as work or school closure, but there might be more subtle and focused cases when the outbreak is still manageable (e.g. avoiding large, close, gathering festivities for example), and people might themselves change their own behavior. In the case of the current China outbreak, for example, Chinese people are privileging the use of more digital life styles, instead of face to face social interactions, while a large part of people stop going out, to restaurants, or stop travelling.7
How large is the contact disease decreasing voluntarily? In fact, contact rates happen at different moments, from work, communities and families, and some are difficult to reduce, e.g. at work, or at home, etc. Most studies suggest that contact rates for non infected individuals, have decreased by 30% to 40% during period of large influenza. A study made from data during the spanish flu waves by 1919 in Sydney, mentioned a reduction of 38% of contacts among the inhabitants, across a set of multiple waves of the flu reappearing.8
3. The baseline of those 5 actions during outbreak: flattening the curve
Deriving the high level math
The five actions above are all good sense, and have been used spontaneously by many, yet neither extensively and intensively, even in the context of a perceived severe infliuenza threat, such as H1N1. We derive hereafter the gain in contagion probability, for the typical extra use observed of each action, and come to the finding that the total extra reach of actions may already lead to a significant decrease in the reproduction rate, \(R_t\).
Effect of washing hands with soap
If we define a base line worldwide, there is roughly 20% extra population washing their hands with soaps, and/or use sanitizers during outbreak, of which 2/3 take the maximal protection measure. In such a case, we assume the lucky rate success of 50% reduction (the 5% lucky winners), so that the proportion of contagion is reduced by 8% worldwide. Likewise infected people protect themselves by washing hands, reducing the probability of contaminating people, by an extra 15%, roughly. Mathematically, we have, that the increase in probability of being contaminated, \(\frac{\frac{dp}{dt}}{p}=\frac{dR_t}{dt}\) goes down, by:
Hence, for an average influenza, with attack rate at 5% to 20%, the extra reach of hands washing, leads to a reduction in contagion between 13% to 20%.
Effect of wearing masks
Mask usage is not that frequent in our population. In the curse of recent, mild, influenza, roughly 10% (30%) of Western European people used masks at start (peak) transmission and roughly half of them do this in fear of catching the virus, while the other half do it to protect their relatives based on their illness, in their home or at work. During the H1N1 outbreak in 2019 in Hong Kong, roughly 25% of inhabitants used to wear masks, but the percentage raised to 80% when going into public spaces.9 The average time a day wearing the mask in public is large, up to 4 hours, in the home, and is thus likely effective.
Taking a rough average of extra protection use of masks out those studies, and the fact that roughly 30% to 40% of infections occur in communities/houses (see my previous post), we can compute the following effects of mask usage:
We can thus compute that, for an average influenza, with attack rate at 5% to 20%, the extra reach of wearing mask, leads to a reduction in contagion of between 5% and 12.5%.
Effect of fresh air ventilation
Typically people spend between 75% to 85% of time inside, and only 50% can leverage fresh air ventilations at work (implying that home refreshing is the main natural domain of contagion reduction). We can compute:
This is an average as we do not know how the behavior is pushed by extent of attack rate. The average influenza leads to an effect of 5%.
Effects from staying home when sick
We refer here as to contaminated person, where 30% extra will decide to stay home despite being at risk of contaminating people. Susceptibility of being contamined depends on close contact and infectiousness during one week. If we beleive that the peak infectiousness is 4 days, and close contact at work is 70% of total contacts, as per multiple studies, then we come the folloiwing reduction. For kids, the decision to remain at home when sick is 10%, thus on average we have:
For an average influenza, with attack rate at 5% to 20%, the extra reach of staying at home instead of going to school or work, leads to a reduction in contagion of between 0.5% and 2%.
Effects from close contacts
The effects on limiting contacts has been seen to be relatively large, in the range of 40% in the case of the 1918 high pandemic flu in Australia, for instance. This reduction rate concerns a three waves outbreak of the disease, affecting 60% of population. Media and information suggests than 60% of those contacts correlate full with outbreak, while roughly 70% of contacts are close enough contacts to be infectious. We can thus infer the following:
For an average influenza, with attack rate at 5% to 20%, lowering contact rate, leads to a reduction in contagion of between 9.5% and 27%.
4. The aggregate picture
The aggregate picture is presented in Figure 1 with the following insights:
-
First, we rank the effects based on their marginal impact on contagion and the typical extra use during pandemics — social distancing, hygiene and face protection measures are three most relevant measures.
-
Second, the reproduction rate of the COVID-19 as measured from Chinese data, quickly went down from 6 to 2.5-3 in one month, and now is likley below 1, or a decline of more than 85%. The below suggests that at potential attack rate of 10%, between 35% to 50% of the decline is linked to spontaneous changes of the Chinese behavior, the balance may hence be due to policy shutdown.
-
Measures effectiveness relatively decreases with attack rate. If we move from 5 to 25% attack rate, of five times more, the probability of being infected decreases by a factor of two for the same level of measures. It is thus critical to play at the start and not wait. And it is thus clear that we need more than voluntary behavior to stop aggressive pandemics.
Figure 1: the likely effect of the 5 behavioral changes on \(R_t\)
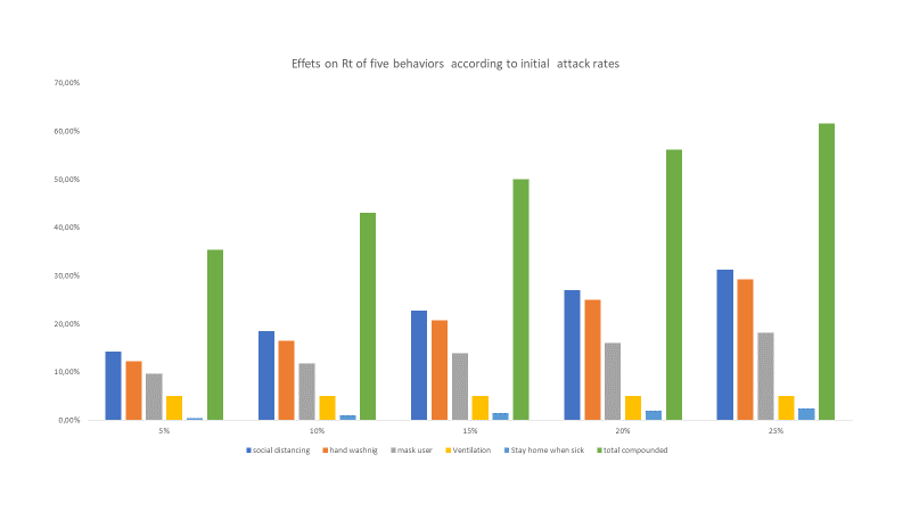
Source: estimates taken from extensive lit search, model, author’s own computation. High level estimates, aggregate estimate suggests 50% overlap among individuals of the 5 actions
5. What else to do
As the above suggests that behavorial changes are powerful to curb infection, but not enough to stop viruses with reproduction rates above two, a set of structural policies must be implemented, such as school closure etc, besides quick discovery of delivery of anviral doses, and of vaccines.
Another path is to push campaigns that really lead a broader use of people of the five behavioral measures above. We can still increase largerly the portion of people who will be washing hands, wearing masks, we can still refrain more close contacts, etc. In effect, the total reach potential may be twice larger what we have; or for the average infleunza, this means we might increase by 50% the effectiveness of the portfolio of measures versus the average to date.
There is a real good news is we ALL to do the tricks. Do not wait and comply.
© Jacques Bughin. Written March 12. Comments more than welcome. All errors are mine. References listed as they are found in the text
-
See Freeman, et al. 2014, Systematic review: hygiene and health: systematic review of handwashing practices worldwide and update of health effects, Tropical Medicine & International Health. ↩
-
See Fleischman et al. (2011), Sensor recorded changes in rates of hand washing with soap in response to the media reports of the H1N1 pandemic in Britain, British Journal of Medicine. ↩
-
See Van Cauteren, D., 2012, Burden of influenza, healthcare seeking behaviour and hygiene measures during the A(H1N1)2009 pandemic in France: a population based study, BMC Public Health. ↩
-
See MacIntyre et al., 2009, Face mask use and control of respiratory virus transmission in households, Emerging infectious diseases. ↩
-
See Offerman, F.J., Robertson, J., Springer, D., Brennan, S. and Woo, T., 2007, Window usage, ventilation, and formaldehyde concentrations in new California homes: summer field sessions, Healthy and Sustainable Buildings, ASHRAE. ↩
-
See De Blasio et al, 2012, Estimating influenza-related sick leave in Norway: Was work absenteeism higher during the 2009 A (H1N1) pandemic compared to seasonal epidemics?, Eurosurveillance. ↩
-
See https://www.bloomberg.com/press-releases/2020-03-04/westwin-research-shows-how-chinese-consumer-behavior-changed-as-a-result-of-the-coronavirus-COVID-19-outbreak ↩
-
see Caley, et al 2008, Quantifying social distancing arising from pandemic influenza, Journal of the Royal Society Interface. ↩
-
See MacIntyre et al., 2009, Face mask use and control of respiratory virus transmission in households, Emerging infectious diseases. ↩