Why we must protect the healthcare workforce during COVID-19
-
-
-
-
J. Bughin
Dr Jacques Bughin, UN consultant, Solvay Business School ULB, Portulans Institute and G20Y, former Director McKinsey Global Institute, and senior partner McKinsey & Company.
1. Introduction
March 18
The COVID-19 pandemic continues its world expansion, affecting now more than 200,000 citizens, and leading many countries in the midst of the turmoil to launch aggressive social distancing plans, constraining multiple business closures, and further adding economic stress, on top of health risks.
Those costs may seem to be large for some people, as indeed COVID-19 does not match the fatality rate of scary diseases like Ebola, and many others, but it is critical to recognize that the level of contagion of the virus is large enough to induce a very large number of fatalities, possibly in an order of magnitude 10 times, higher than what we usually have observed with the normal flu. Last but not least, a burst in the pandemic may quickly overwhelm health systems, leading to much larger fatality rates for those 20% of serious COVID-19 infections, which either may be denied access to hospitalization, or may be hospitalized with sub-optimal care (emergency unit overflows, etc).
The importance of enough technical capacity of healthcare is thus critical for managing the COVID-19 epidemic as recognized by many. But the healthcare workforce must also be fit as well. A burst of the disease would imply for the health professionals ascending workload, exposure to stress, possible violence by patients, or simply large and not fully safe exposure to the outbreak.
As the Spanish and Italians confined in their house and apartment buildings were applauding health workers for their commitment in recent days, all of us should also do the same. We should also try to avoid scenes seen in Wuhan as late January when hospital capacity quick came short, and timely treatment being denied to (suspected to be) contaminated, leading to direct violence towards the healthcare workforce. The solution there was to build capacity in less than 10 days, and reallocate health resources to the Hubei region. Not known enough, a large part of health professionals also volunteered to come to help, another sign of strong ethics of the healthcare professionals, seen in other exceptional settings such as the various bombings in recent years and the 9/11 attack.
In this article, I look at, and try to provide some quantification of the burden of health workers during outbreaks. Our finding suggests that the heavy lifting seems to be large, and healthcare workers must be prioritized and supported during and after the outbreak.
2. How healthcare professionals are affected: up to 5 times more disorder, and fatalities
Besides possible violence, there are multiple negative channels that affect healthcare professionals. Let us take two main ones:
Psychological pressure: three times more frequent for healthcare professionals during outbreak than population
The first is large psychologic pressure. In a recent study on how healthcare felt during the exponential growth of cases in Wuhan, there is clear evidence that stress level is relatively high during such an outbreak.1 Close to 4 out of 10 healthcare workers were in a situation of clinically diagnosed psychological distress during the exponential growth of the disease in early February in the region, and the percentage of stressed workers was close to 50% in the most affected city, Wuhan. This is typically 3 times the rate of the population, and possibly more than two times the rate of healthcare workers.2
Looking deeper at the data, there is clear evidence that stress is highly correlated with the fact of being in the frontline, participating in treatment, especially as a doctor or nurse, and especially if the worker is aware of any family members, or colleague being affected (See figure 1).
Figure 1: over-stress of healthcare workers during the COVID-19
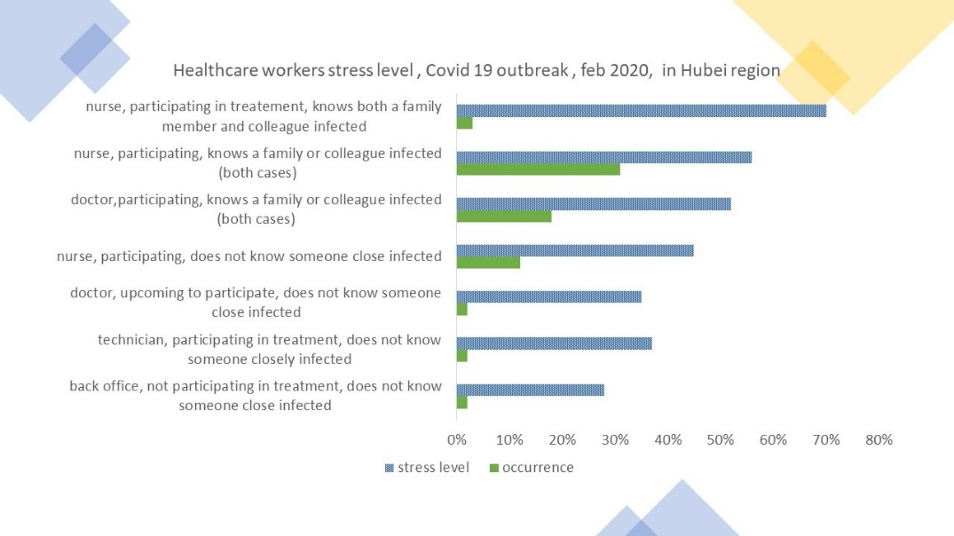
Further, by recrossing the data set, half of the most affine health professionals where in situation of major stress when caring for COVID-19 patients. This is similar to other results in Hong Kong, during the SARS with 57% of healthcare professionals were facing large distress.
Morbidity afflictions: 5 times more exposure for healthcare professionals during major outbreaks
The story of Dr Li Wenliang, who had tried to warn, but was rebuffed by, the authorities of Wuhan on the danger of the outbreak, to become infected by the virus and who passed away in February is a clear reminder that health professionals are at higher risk of contamination and worse.
There are many causes of accidents and mortalities linked to various occasions, e.g. a driving accident for truck drivers, bad sea weather for fishermen, or falling trees for lumber jackets. In the US, for example, the CDC reports that there are about 3.5 deaths a year for 100,000 workers, or roughly 5500 deaths, outside of infection related; construction workers and fishermen will be much larger than that, as well as truck drivers. The rate is good for healthcare professionals, yet with a wide range, 4 times more for physicians than home nurses, and 8 to 10 more than home nurses, for those working in the emergency room.
Infections are nevertheless the largest cause of death at work, if one adequately traces causes of death from major diseases such as cancers, and cardiovascular disease.3 Zooming on communicable disease for our purpose, the statistics, while very imprecise, seem to suggest that healthcare professional may be subject to fatalities, more than 2 times the average work occupation in the US (Table 1). The front line healthcare workers get about 2.5 times more fatalities than the average US workplace.
Table 1: Fatalities in the US, estimates
| Death from activity | Death from communicable disease (only) | |
|---|---|---|
| Total workforce | 5,500 | 2,300 |
| Healthcare professionals | 80 to 100 | 150 to 300 |
| Ratio of death | 1.4% to 1.6% | 6.5% to 13% |
| Share of healthcare professionals in workforce: | 3.7% to 5.5% | |
| Odd ratio | 30% | 1.8 to 2.3 |
Source: ILO, CDC, lit search, own computation
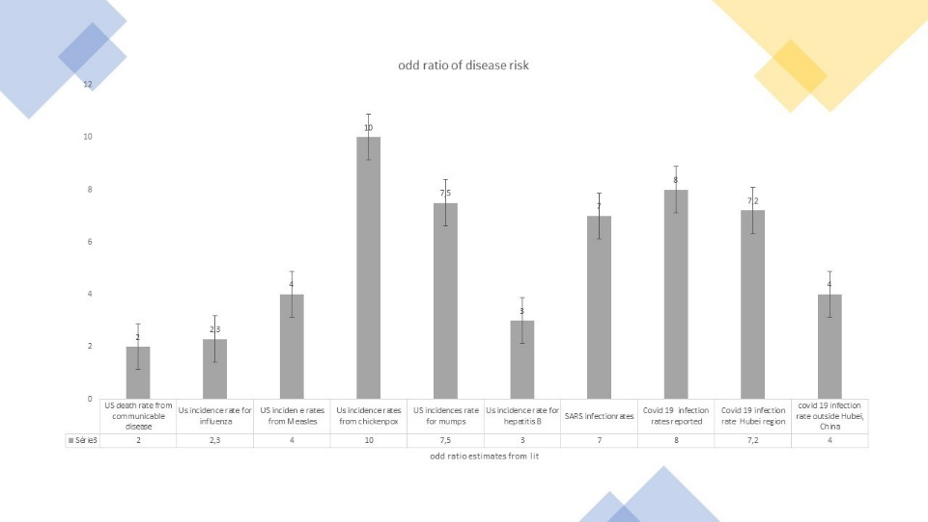
Those odds ratios against health professionals can be triangulated with disease specific cases, with a clear message that tens of infections have been transmitted to healthcare workers, including measles, varicella, and others. Outbreak-associated attack rates have been in the range of 15% to 40%, or roughly two to three times the rate of the population.4 Odd ratios in this case have been computed for contamination, as death rates are very complex to gather:
-
Influenza typically boosts absenteeism by 30% for the average workforce population, it is 70% higher for hospital nurse, or a odd ratio of 70/30 = 2.3.
-
For tuberculin skin test, 5% of US population was tested positive, for up to 40% for urban healthcare professionals, or an odds ratio of 8.
-
Of all US healthcare professionals, 1% to 2% could get chickenpox, while the rate is close to 10 times lower in the US in the nineties.
-
Healthcare workers were the sources of close to 10% of all cases of measles, while representing 5% of workers, and 2.5% of total population.
-
15% of physicians used to get mumps, for 2% average of population.
-
US incidence rate is 6 (per 100,000) among healthcare professionals, or about 3 times the incidence in the total population.5
Those statistics are for the average communicable diseases. What do we know for (more exceptional) outbreaks?
-
Regarding SARS and MERS, it was reported that 21% (19% respectively) of the cases were linked to health care workers, representing 3% maximum of population, of an odd ratio of 7.6
-
Regarding COVID-19, reports suggest that more than 3,000 healthcare workers got infected by early February 2020 in China.7 As there were about 60,000 professionals dispatched in Wuhan, and Wuhan was 70% of the outbreak in China at that time, this might suggest that \(0.7\times\frac{3,000}{60,000}\), or about 3.5%. Other research implies that reported infection in the Wuhan region by healthcare professionals was 2.5 percent.8 If one believes the Chinese statistics on reported cases, and Wuhan inhabitants is 11 million, the infection rate in the city is more like 0.3 to 0.4 percent, leading to an odd ratio of 6 to 10. The same research in Dai (2020), shows that healthcare knew 5.7 more colleagues infected than family infected in the Wuhan region, 7.2 times more in other regions in Hubei, and 4 times more in other provinces, reporting same odd ratio as other sources, but showing the the odd ratio is larger in most exposed regions. This is because the outbreak happened in the Hubei region and the Chinese authorities got ill prepared at the start, exposing the healthcare professionals more than they should have (Figure 2).
Figure 2 - Estimated odd ratio of disease exposure for healthcare professionals
3. Why more exposure and distress?
What brings such high exposure risk and distress? The first reason is that most of the hospitalization visits have higher chance of being contaminated, and if so, the contamination may be already for patients in risky health conditions. Otherwise stated, there is a large selection bias of sick people with a high contagious disease. This leads to a significant higher odd ratio of being affected, and a stress risk of the professional being likely infected (for 40% of workers).
One interesting thing is that the largest worries are typically altruistic, e.g. infection of colleagues (more than 7 out of 10) or of family ( for 2/3 of them).9 Another crucial root cause of the stress was the logistic aspect and enough protective measures being implemented. Such shortages were prevalent in the first weeks of handling the outbreak in Wuhan, and were significantly adding to distress.
4. A mandatory roadmap
Hence, we have shown that risk and reality are high and match, making healthcare professionals quite aware of the danger of their jobs during outbreaks. Remarkably, 90% face those risks, with only 10% would hesitating to show up for work, and a large part would even like to volunteer. Given the risk they take, their altruistic behavior during those difficult period, and the fact they can save our lives, we must absolutely make sure that all is done to alleviate their effort, reduce their distress, and ensure best healthcare. This goes hand in hand with a non negotiable plan with at least those requirements:
-
Make sure to support the difficult journey through psychological squad teams. China has some good practice here - psychological intervention teams have been set up to cover the full workforce, with four action items. A psychosocial response team coordinates the management team’s work; then a psychological intervention technical support team build a psychological intervention material and design rules. Thirdly, a medical team, with psychiatrists, participates in clinical intervention for healthcare workers. An assistance hotline team provide remote advice to deal with mental health problems. Hundreds of medical workers are receiving these interventions, with good response, and their provision is expanding to more people and hospitals.
-
Ensure a sufficient supply of protection for everywhere use in hospitals. This is a major concern, and this must be in enough supply to cover not only hospital beds and emergency rooms, but when patients come to the hospitals, etc. There is always the tension that supply is short, because of cumbersome commissioning procedures, etc. It is important that the governments quickly found and leverage other citizens initiatives and local sources, to build masks, protection etc.
-
Define beta protocols and refine along the way to treat patients. With a new virus, and outbreaks may come chaos, and confusion. It is imperative that protocols are set up in great details and ingested by all heathcare workers - this will save stress, live, and will help healthcare workers with clearcut instructions and a sense of being taken care of, in order to cope better with the outbreak. This has proven very valuable during previous outbreaks like SARS.
-
Focus on health, it is an investment. Healthcare has large positive externalities, save days at work, and life. Thus this should be the mission, and the authorities should make sure the rest is not priority and is not of a concern for healthcare professional - if they put at risk their time, they should be paid accordingly.
-
Thank them and show gratitude. I take this occasion to applaud their journey just right now - and will make sure my voice is heard that they deserve the best energy and recognition, without pain points, to make us pass through this outbreak. Thank you.
© Jacques Bughin. Written March 18. Comments more than welcome. All errors are mine. References listed as they are found in the text
-
See Dai, 2020, Psychological impact of coronavirus disease outbreak on heatlhcare in China, MedRix, and Fang, 2020, The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus, The Lancet. ↩
-
See e.g. Wang et al, 2019, Study on the mental health status and infliuencing factors of chinese medical teams, Zonghua. ↩
-
See ILO work and recently https://www.who.int/occupational_health/activities/occupational_work_diseases ↩
-
See e.g. Sepkowitz , 1996, Occupationally acquired infections in health care workers, American College of Physicians. ↩
-
See Kim, 2009, The epidemilogy of Hepatitis B inthe US, Hepatalogy. ↩
-
See Park et al., 2018, MERS transmission and risk factors: a systematic review, BMC Public Health. ↩
-
See Walls, 2020, Supporting the healthcare worlfoce during the Covd-19 global epidemic, JAMA. ↩
-
See Dai, 2020, Psychological impact of coronavirus disease outbreak on heatlhcare in China, MedRix. ↩
-
P.S.: The risk of colleague scores higher, not because, workers do not like their family, but because they were in an environment were the risk is decoupled, and in effect, workers in healthcare services at Wuhan knew 6 times more often a colleague being affected than a family member. ↩